Ultrasound
Calendar Method
Ultrasound examination, even though quite frequently used nowadays, is not at all simple. Ultrasound of two organs, uterus and ovaries, can sometimes be rather complex and difficult to interpret. The reason is that uterus, it is lining, and ovaries significantly change their morphology and characteristics depending on the following:
1. Woman’s age
- Childhood
- Adolescence
- Generative age
- Postmenopause
2. Phase of the cycle
- Proliferation / follicular phase (first phase of the cycle)
- Ovulation
- The luteal phase of the cycle
For higher resolution ultrasound, only a probe with a frequency of 7-10mHz is used in gynecology. In a longitudinal section, you can see a top (fundus) of the uterus, a body, and a cervix. The longitudinal section goes along the mid axis, i.e., through the mucosa, whereas the cross-section can be set anywhere across the uterus.
The endometrium is thin during menstruation. That simplifies diagnosing intrauterine pathology – polyps, myomas, and synechiae. Therefore, most gynecologists prefer ultrasound examination during or immediately after the period. Later in the cycle, all the way to the ovulation phase, the endometrium thickens.
A so-called triple-line endometrial pattern characterizes ovulation. This comes from creating so-called luteinized cells and the thickened endometrium, resulting from progesterone production in the ovulating follicle. At a later stage, when luteinized cells fill the whole endometrium, the endometrium becomes hyperechoic throughout. This finding is characteristic for the late secretory, or luteal phase, and represents a relatively accurate indirect proof of quality ovulation.
Polyps are common pathology during the generative age. They are rarely found on ultrasound by chance; a woman usually has characteristic symptoms – sudden irregular, prolonged and heavy bleeding, or inability to conceive. They are most accessible and best seen during menstruation as they are clearly marked by hypoechoic blood.
The uterine septum is a congenital uterine malformation. The size can vary from a minimal, when referred to as uterus arcuatus and uterus subseptus, to malformation when a uterine cavity is partitioned by a longitudinal septum going all the way to the cervix. It is well known that a minor septum causes significant problems during pregnancy. A conventional ultrasound can raise suspicion of the uterine septum, but a definite diagnosis can only be established through a 3D ultrasound, HSG, or hysteroscopy.
Myomas are common pathology. There are submucous myomas which, regardless of their size, mainly cause irregular bleeding as they are found in the uterine cavity; intramural myomas, which should be monitored as they can grow without symptoms, or cause irregular bleeding, have secondary changes, become painful and alike; and subserous myomas which are lumps that protrude toward the abdomen.
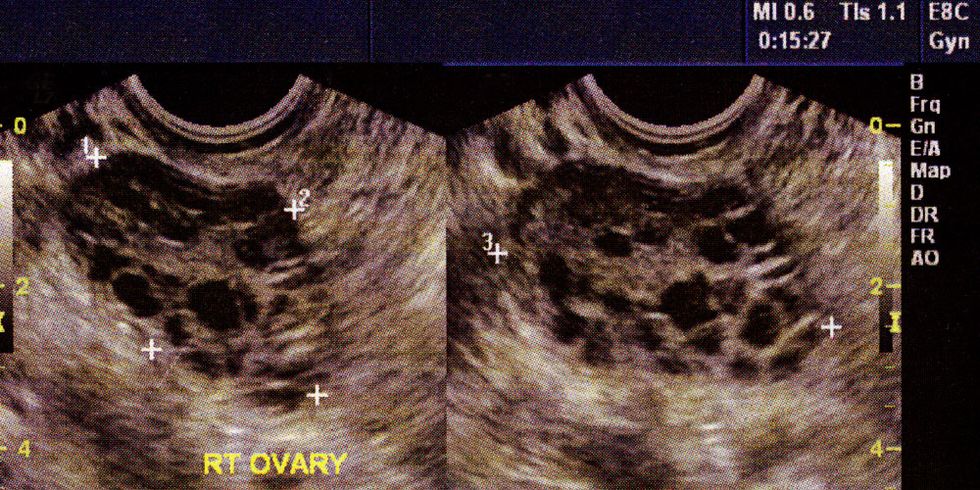
The normal ovary is situated freely in the pelvis during the fertile period, with stroma and follicles visible. In each stage of the cycle, both ovaries host several follicles sized up to 10mm. These so-called antral follicles go into atresia if not chosen to be a leading follicle in that cycle.
In the late proliferative phase, a leading follicle is developed. From the moment it was chosen as the leading follicle, which can be seen by ultrasound when it reaches the size of about 10mm, to the ovulation, it grows at the rate of 2-3mm a day. Ovulation occurs when such follicle reaches 22-28mm.
Every ovulation leads to a certain amount of bleeding in the wall of the ruptured follicle. The ruptured follicle becomes corpus luteum that, three days later, transforms into corpus luteum. The Corpus luteum sustains the other half of the cycle in hormones, thus preparing the environment for a potential pregnancy. In order to be successful, it requires an exceptionally supple blood supply.
Ovarian pathology
Cysts quite frequently develop in the ovaries. Typical are functional ovarian cysts that can be follicular or luteal, with smooth walls and clear, hypoechoic liquid content. They can reach even 10cm in size. In over 90% of cases, they will spontaneously resolve after a 2–4-month period; therefore, it is a mistake to refer such a patient for surgery immediately. Monitoring is all that is required.
What can be misinterpreted as a functional cyst is fluid in the Fallopian tube. Sactosalpinx or hydrosalpinx is a term for altered Fallopian tube, which is usually twisted around its axis, so cysts are visible in the transverse section through the structure. We can only be certain we see the tubes is to notice an ovary next to a cystic formation, which is not always easy.
Some cysts have no smooth walls or clear liquid contents, such as bleeding corpus rubrum or CRH (corpus rubrum hemorrhagicum). Inside the cyst, there is a content that is characteristic for fresh intraovarian bleeding. Of course, when a woman comes with typical clinical features of sudden pains arising at ovulation and typical ultrasound finding, it is easy to determine a diagnosis. In about 10% of cases, CRH requires a surgical procedure – if the bleeding will not cease (i.e., if CRH increases) or if corpus rubrum bleeds into the abdomen (can be identified by the loose liquid in the abdomen) if the pain is extensive. If no surgery is necessary, CRH will spontaneously perish.
Endometriosis is another frequent, but unfortunately, severe condition of gynecology. It consists of cysts with thick walls and so-called chocolate content, which is essentially old blood. There are flow-through cysts walls, and it is usually of low resistance index (RI) – it can go as low as 0.40. As endometriosis is accompanied by elevated tumor marker of coelomic epithelium, CA 125, it is easily confused for malignant conditions.
Ultrasound can also determine ovarian reserve (AFC – antral follicle count), which is very important when determining pregnancy chances in infertile women.





.jpg)





.jpg)

